
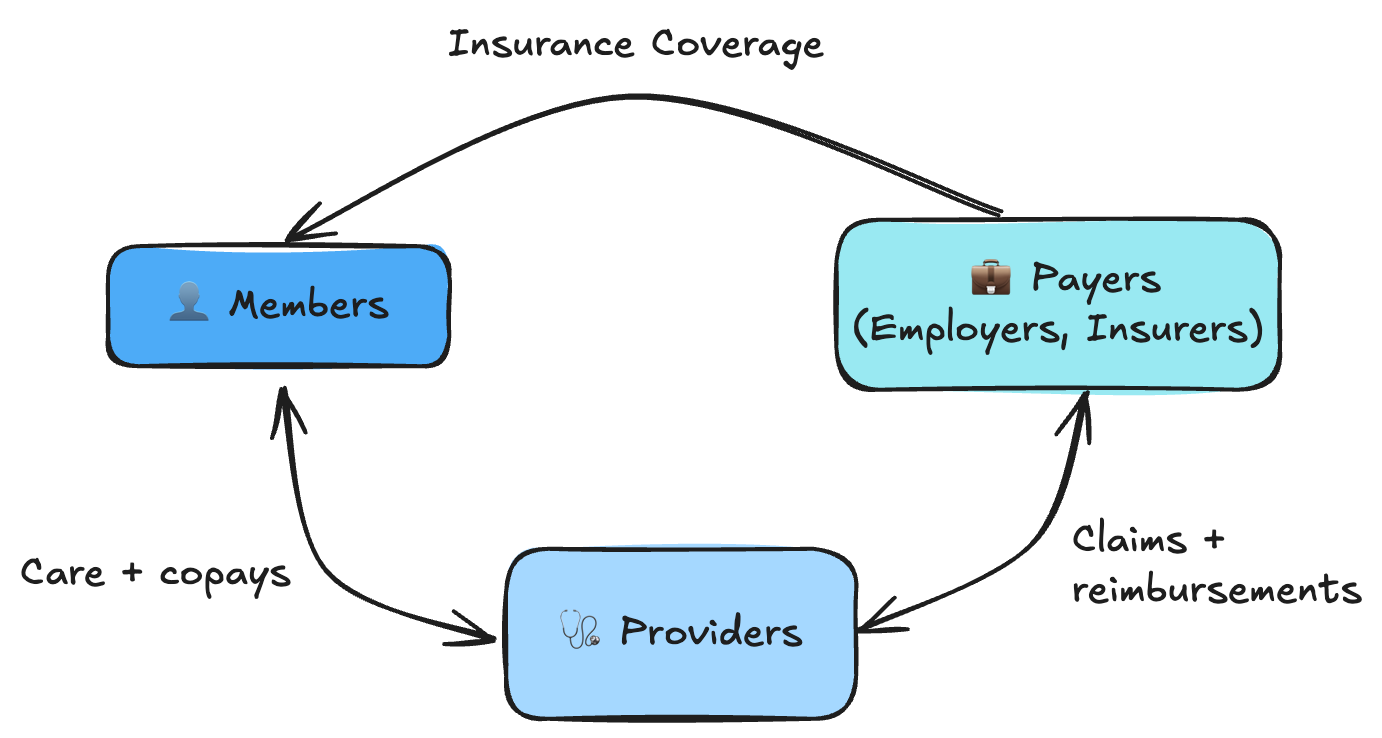
They are already working with payers representing tens of thousands of members, giving them access to more affordable and transparent care options.
Founded by Deep Kapur & Louise Tanski
They both went to Penn and later worked together at Rupa Health, where they saw firsthand how outdated health insurance infrastructure makes it nearly impossible to deliver affordable, flexible coverage.
They are second time founders that have built and exited companies in workflow automation and healthtech, and spent months working with payers and plan administrators before starting Amera to rebuild the foundation healthcare runs on.

Health insurance costs are rising twice as fast as inflation. American families now pay over $30,000 a year for coverage they’re unhappy with. 160 million Americans get insurance through their employer, and to control these costs, many large companies (>250 employees) self-insure - they pay employees' medical claims directly instead of buying traditional insurance from carriers like UnitedHealth or Cigna. But the infrastructure powering these plans is decades old - some core systems still run on COBOL. This legacy stack makes operations manual and expensive, blocking adoption of affordable plan designs or AI-driven automation that could lower costs.
Amera converts messy claims data from any source into structured data that existing systems can use. From there, they automate repetitive back-office work - validation, reconciliation, and stop-loss reporting - cutting manual effort from hours to seconds and making the processes transparent for the first time.
Why is this hard? Health insurance tech has loose standards. Every plan runs on bespoke systems that cannot talk to each other. Claims arrive in hundreds of formats - EDI, PDFs, fax, proprietary systems - making automation nearly impossible without a unified data layer.
They have built the most comprehensive set of schemas for healthcare docs, designed to map to hundreds of custom formats and be fully interoperable. This makes it easy for them to layer new automation on top of existing systems.